HEALTH AND EU ACCESSION:
SOME CHALLENGES TO THE USE OF HEALTH IMPACT ASSESSMENT
IN HUNGARY
Margit OHR
International Policy Fellow
Contents
- Acknowledgements
- Summary of findings and recommendations
- Introduction
- Policy research questions
- Methods
- Health Impact Assessment in the European Union
- Development of HIA in Europe
- The EU Public Health Programme
- HIA in the EU
- Case studies
- HIA in the UK
- HIA in the Netherlands
- Situational analysis in Hungary
- Policy context in Hungary
- Factors affecting use of HIA in Hungary
- Comparison of factors affecting HIA in Hungary and the EU
- Conclusions and policy recommendations
- Establishing a legal framework for HIA in Hungary
- Building capacity
- Institutional development
- References
Tables
1. Factors affecting the use of HIA in Wales
2. HIA’s coordinated or produced by NSPH
3. Factors affecting the use of HIA in Hungary
Figures
1. Key stages in HIA
2. Perceived barriers to using HIA in government policymaking in European
countries
3. Comments on HIA made by Tessa Jowell MP [former] Minister of State
for Public Health
4. main objectives of the Dutch plan of action to develop HIA in 1995
Acknowledgements
I would like to thank the Open Society Institute International Policy
Fellowship Program for awarding me a Fellowship that enabled me to
carry out this policy research study. In particular, Pamela Kilpadi
(IPF Program Manager, Mladen Momcilivic (IPF Program Coordinator)
and Csilla Kaposvari (Public Health Fellows Coordinator) gave me support
and encouragement during my fellowship year (2002/2003).
I would like to express gratitude to my mentors (Hungarian
mentor: Dr. Mihály Kökény, Parliamentary Secretary
of State, Ministry of Health, Social and Family Affairs; International
mentor: Dr. Martin Birley, Director, International Health IMPACT Assessment
Consortium, University of Liverpool). Both gave me their time and
helped to inform the development of my research and access to networking
and training opportunities. In addition, Dr Birley facilitated my
involvement as a third party in a current EU-funded (SANCO) project:
Policy Health Impact Assessment for the European Union.
I am grateful to all of the people I interviewed for
their willing participation and interest in the research.
Mention must also go to Ceri Breeze of the Public Health
Strategy Division, Welsh Assembly Government, for involving me to
the Pan-European HIA Survey 2002 and to his colleagues Heather Giles
and Marc Boggett for they support of these work.
Finally I would like to thank to Edit Sebestyén
(health promotion expert) for her research assistant work that helped
me to carry out this work.
If readers have comments or feedback on this paper,
please contact me at ohr@policy.hu
Summary of findings and recommendations
Introduction
This paper is one outcome of my research work within the International
Policy Fellowship Programme of the Open Society Institute, Budapest,
Hungary during the 2002/2003 fellowship year.
The paper discusses opportunities and barriers to the
use of Health Impact Assessment in Hungary and makes some key policy
recommendations relating to the implementation of HIA in the context
of EU Accession.
The paper starts by providing some relevant background
on the use of HIA in the European Union and then presents more detailed
case studies based on experience of using HIA in the UK and The Netherlands.
It then goes on to identify and assess the current situation in Hungary
with particular attention to opportunities and barriers to understanding
and using HIA.
Aims and objectives of study
This study is the first step to look at and analyse all the significant
factors that can be supportive and barriers to the implementation
of HIA into the national decision making process. The aim of the study
is to identify these factors and by dealing with them prepare the
ground for capacity building for HIA.
Key findings
The key findings of this study relate to the following categories:
evidence, political/policy, institutional and resources. Examination
of the use of HIA in the EU and especially for this study, in the
UK and Netherlands, show that there remain significant barriers to
the use of HIA. However, the policy context is broadly supportive
of efforts to use HIA in both the UK and Netherlands. For example,
key policy drivers are: evidence-based action, intersectoral responses
and community participation in policy and planning, to complex policy
challenges (poverty, sustainable development, health inequalities).
By contrast, in Hungary:
- there is understanding of the complex policy challenges facing
Government. However, policy design and critically, implementation
is still pursued through sectors and sectoral interest groups
rather than developing more flexible, intersectoral means of both
identifying, designing and delivering action. In part this reflects
a lack of investment in modernising public administration, especially
in the health sector
- relatedly, an evidence-based working culture is not widespread
in policy and professional arenas
- finally, policy and strategy is still largely developed by
small closed groups of expert and bureaucratic interests lacking
transparency and meaningful engagement with wider stakeholder
interests.
The assumption informing this research was that EU Accession would
stimulate some of the changes necessary to modernise policy making/public
administration and enable the adoption and development of relevant
methods such as HIA. So close to EU Accession, this research shows
that in Hungary commitment to and investment in dealing with
policy and public administration development e.g. as a platform for
applying HIA methodology, is not obvious. Effective capacity building
will need educational, institutional and strategic level investment,
not least to tackle all the political and more seriously, the institutional-cultural
barriers to development.
Recommendations
The main recommendations are given below.
- Developing capacity and confidence in HIA should be part of
a broader effort to modernise policy making and institutions in
Hungary
- Carrying out HIA should be an essential part of government
planning and decision making in order to place health in the centre
of the decision making process.
- Under the Hungarian system, the requirement for HIA should
be regulated by law with clear lines of accountability through
the Minister for Health, Social and Family Affairs ultimately
reporting to Parliament
- Developing capacity (strategic, institutional and educational)
for HIA should be championed by the ‘modernising’ centre of gravity
in the Hungarian Public Administration
- Responsibility for guiding implementation of HIA across Government
should be located in a background institution working mainly in
relation to the Ministry of Health, Social and Family Affairs,
Ministry of Finance and the Prime Minister’s Office.
Key words: modernisation, health impact assessment, policy,
barriers, opportunities, comparison, capacity building, Gothenburg
Consensus statement, England, Scotland, Wales, Hungary, good practice,
Netherlands, European Union, World Health Organization
1. INTRODUCTION
EU competence in health is not limited to simply to activity labelled
health or public health. Under the terms of the Amsterdam Treaty,
there is a specific requirement that
a high level of human health protection be ensured in
the definition and implementation of all Community policies and
actions (Article 152)
This means that a broad range of activity (e.g. related to the Internal
Market, structural funds, social affairs, social inclusion, agriculture,
the environment, trade and development policy) must be appraised for
its potential impact on the health and well being of EU citizens.
Hungary is expected to join the EU in May 2004. In this
context the purpose of the work reported in this paper was to explore
factors that might affect the use of Health Impact Assessment in Hungary.
Two main sources of information inform this paper: (i) published experience
from among EU member states and (ii) findings from indepth interviews
with Hungarian stakeholders.
The ultimate goal of this work is to contribute to first
steps to build capacity within the Hungarian system to conduct health
impact assessment of any relevant policy or programme at national
level .
1.1 Policy research questions
The following research questions were identified at the start of the
Fellowship and then explored during the year:
- What might be considered as good practice in health impact
assessment?
- Do stakeholders in Hungary currently consider the health
impacts of, especially, non-health sector policies?
- Is the requirement for HIA considered, as a consequence
of EU Accession?
- What capacity and capability exists within Hungary to
use HIA methods as a systematic means of appraising the potential
and actual health impacts of policy?
- What actions could be taken to improve understanding,
confidence and expertise in HIA in Hungary?
1.2 Methods
The research process and methods used are summarised
below:
Review of HIA methods and practice:
- library and internet searches (February-March
2002)
- participation in IMPACT training course
(Liverpool, April-May 2002)
- participation in a Department of Health
meeting for EU Accession Countries to look at public health development
needs (London, April 2002)
- participation in IAIA Conference (The
Hague, June 2002)
- third party participation in EU (SANCO)
funded project: Policy Health Impact Assessment for the EU (August,
2002)
- Hungarian respondent to the Pan-European
HIA Survey (April 2002)
Situational analysis in Hungary:
- in-depth interviews with Hungarian
stakeholders (n=10 representing - Ministry of Health, Social and
Family Affairs, National Public Health and Medical Officer Service,
Universities, National Governmental Agencies, Ministry of Environment,
local experts and other professional colleagues) (Budapest, April-December
2002)
- development of policy briefing paper
on HIA for Parliamentary State Secretary at Ministry of Health,
Social and Family Affairs (Budapest, June, 2002)
- membership of an Advisory Group on
Capacity Building for Public Health convened under the National
Public Health Programme (Budapest, October 2002)
As the above diagram implies, it was sometimes hard to distinguish
between the policy research project, professional development and
participation in the policy process at both Hungarian and EU level
during the Fellowship year. Understanding of health impact assessment
and its application was developed through examining available literature
and by the opportunistic use of professional development and networking
opportunities identified during the fellowship year. Paralleling this
were opportunities to inform policy and programme developments in
Hungary and to access networks of key national and local stakeholders
developed over the previous eight years of working at a national agency
in Hungary.
The Hungarian data was collected by interviews with
key Hungarian stakeholders and published and unpublished public health
policy documents. I couldn’t use the survey methodology, like other
European countries in the Pan-European survey, because Hungary was
not in the position to answer for the questionnaire in details. But
I could use the questionnaire as an interview guide for my in-depth
interviews. The questionnaire was structured around several key themes:
• Broad policy context
• Awareness and understanding of health impact assessment
• Use of health impact assessment to date
• Other approaches and other forms of impact assessment
• Issues related to developing further the use of health
impact assessment
I asked the respondents to feel free not the answer
for those questions that are not relevant to them. All interviews
were conducted in Hungarian and they were then fully transcribed.
The resulting transcripts were read several times to better understand
the information being provided by informants. After this, the transcripts
were examined again to identify shared and different issues. These
were then grouped under opportunities and barriers categories for
further analysis. For more in-depth analysis I created new sub-categories:
evidence, political/policy, institutional, resources and I did comparison
with the Wales data as well.
2. HEALTH IMPACT ASSESSMENT IN THE EUROPEAN UNION
This section provides some background to the development of HIA in
Europe and especially the legitimacy and requirement for HIA given
by the European Union in its conduct and the conduct of member states
and pre-Accession countries.
2.1 Development of HIA in Europe
The development of HIA in Canada, Europe and elsewhere was facilitated
by the emergence and acceptance of now overwhelming contemporary (and
historical) evidence that
- historically, the greatest improvements in people’s health
have come not from the health sector (important as this sector
is in supporting health improvement) but from social and economic
changes that improve the quality of people’s lives (Ziglio et
al 2000; Levin and Ziglio 1996)
- currently, the social environment and economic conditions
are a major influence on health status and outcomes at individual,
community and population levels (e.g. Leung and Wong, 2002; Lavis
and Sullivan, 1999; Marmot and Wilkinson, 1999; Gillies, 1998;
Blane, Brunner and Wilkinson, 1996; Wilkinson, 1996).
What this means is that the health care sector has less impact on
and responsibility for changes in mortality, morbidity and other health
status indicators than perhaps the public and many politicians had
thought.
Work by the WHO Centre for Health Policy (ECHP Policy
Learning Curve Series 2001, Number 4; 2001, HIA Discussion papers
Number 1) and others (e.g. OECD/PUMA 2000, Cabinet Office 2000) demonstrate
that in many countries there is understanding that proposed policy
decisions in one sector may impact on outcomes in other sectors. For
example, this has lead in some countries to the development of tools
and methods to assess the impact of economic and social development
policy decisions on the environment. The purpose of such an assessment
is to: improve knowledge about the potential or actual impact of a
policy or programme; inform decision makers and any affected communities;
and enable changes to be made to proposed policies/programmes in order
to help manage negative impacts and promote positive impacts.
Building on experience and learning from environmental
and social impact assessment work, there has been increasing interest
in health impact assessment. Development of HIA has varied according
to circumstances in different countries and the interests of early
champions. For example, in the UK HIA was developed and applied at
local level with little national coordination and application in contrast
to its development in The Netherlands.
This fragmented pattern of development led to understanding
of the need to develop a shared understanding about the core features
of HIA through an international exchange of experience and innovation.
An event in Sweden in December 1999 produced the Gothenburg Consensus
Statement on Health Impact Assessment. According to this statement,
HIA is defined as
Health Impact Assessment is a combination of procedures,
methods and tools by which a policy, program or project may be judged
as to its potential effects on the health of a population, and the
distribution of those effects within the population.
The important common elements of HIA were also set out (see Figure
1).
Figure 1: Key stages in HIA
- screening the potential policy or
programme for linkages with health. If the available information
is limited then the scope of further action has to be agreed
- scoping of HIA which helps identify:
which potential (in)direct health impacts of the policy/programme
need to be better explored; for which specific population
groups; using which methods; resources; who takes part; and
over what timeframe
- appraisal of the HIA report which
may lead to request to add information and reappraisal
- action adjusting the proposed decision
or intention therby acting on the results of the HIA
- monitoring and evaluation of expected
impacts.
2.2 The EU Public Health programme
The new EU Public Health Programme (2003-2008) was implemented on
January 1, 2003. It is a key instrument underpinning the development
of the Community’s Health Strategy. The main objectives of the new
EU Public Health Programme are:
- to improve information and knowledge for the development
of public health
- to enhance the capability of responding rapidly
and in a coordinated fashion to health threats
- to promote health and prevent disease through addressing
health determinants across all policies and activities.
To accomplish these objectives the Programme is intended to contribute
to:
- ensuring a high level of human health protection
in the definition and implementation of all Community policies
and activities through the promotion of an integrated and
inter-sectoral health strategy
- tackling inequalities in health
- encouraging cooperation between Member States in
the areas covered by Article 152 of the Amsterdam Treaty
The Programme will rely on work in four main areas: cross cutting
themes, health information, health threats and health determinants.
Health impact assessment is an example of action required within the
cross cutting theme element.
2.3 HIA in the EU
Despite growing investment in and understanding of HIA methods and
tools (see 2.1 above) relatively little was known until recently about
the application of HIA within the EU. To inform the future development
of health impact assessment within individual member states as part
of the European Community’s Public Health Programme (see 2.2 above),
a pan-European survey of health impact assessment at national government
level has been undertaken. The survey, which covered EU Member States,
accession States and European Economic Area countries, examined perspectives
on, and use of, health impact assessment at national governmental
level. The survey explored the barriers that exist or may be encountered.
The following diagram summarises the results (Breeze C, 2003, in press)
Figure 2: Perceived barriers to using health impact
assessment in government policymaking in European countries
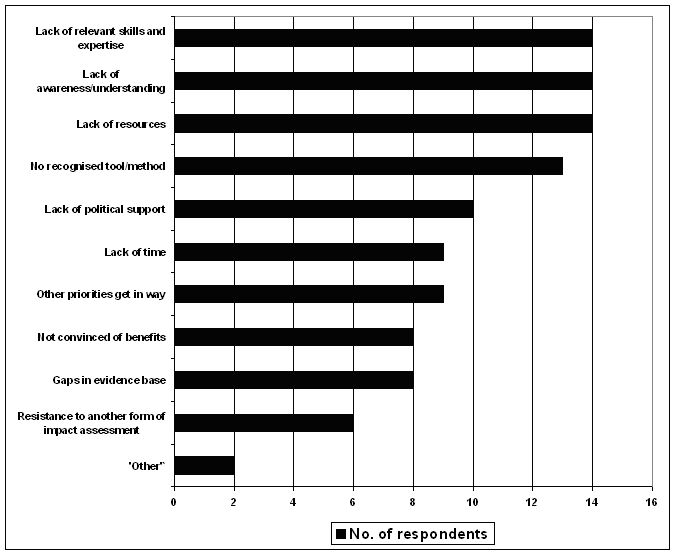
Source: Welsh Assembly Government, 2002
What Figure 2 shows are two main types of problem in getting HIA
accepted and used as part of the policy process: (i) lack of understanding
of the need for and benefits of using HIA (ii) lack of capacity (skills,
expertise and resources and methods). These findings seem surprising
given the weight of evidence outlined in 2.1 above. They suggest a
need to improve the sharing of knowledge and expertise between academic/professional
experts and policy makers and the need to invest in HIA as a normal
part of the policy making process. Recognition of the need for HIA
in the new EU Public Health Programme and the linkage between a broad
range of Community competencies and health in the Amsterdam Treaty
should support wider adoption of HIA.
3. CASE STUDIES OF HIA IN THE UK AND NETHERLANDS
This section provides a more detailed look at two
contrasting developments of HIA, in the UK and in The Netherlands.
In both countries HIA has been developed and applied pragmatically.
However, the most significant difference between the two has been
the use of HIA at local/regional level in the UK and the more systematic
funding and use of HIA at national level in The Netherlands.
3. 1 HIA in the UK
In the UK, public health professionals and academics were early advocates
for HIA (Scott-Samuel 1996; Birley 1995). However, in the absence
of a statutory requirement for HIA to be conducted in specified circumstances,
its development has been patchy and fragmented. This is further limited
by the division of the UK into four main territories (England, Wales,
Scotland and Northern Ireland). In each part of the UK, HIA has developed
in slightly different ways, although people engaged in HIA work exchange
information and experiences through relevant academic and policy networks
common to the whole of the UK.
Figure 3: Comments on HIA by
Tessa Jowell MP, [former] Minister of State for Public Health (England,
UK)
- There is a need to develop guidance
to help other [non-health] government departments carry out HIA
to ensure consistency; that the methodology is simple and non-bureaucratic
as possible, yet at the same time the information that is needed
is properly collected (1998).
- Public health has been weakened by
the lack of evidence that supports judgements and decisions about
policies in so many areas. HIAs can underpin and give integrity
to decisions where that has been lacking in the past, so can provide
a very important tool in building the evidence base [for public
health] (1998).
In 1997, the current Labour Government was elected for its first term
in office and was keen to ‘promote the use of HIA as one aspect of
its agenda to modernise and ‘join-up’ the policy making process in
order to tackle complex issues such as poverty, social exclusion and
public health’ (DoH 1999). An early example of HIA guidance in this
new policy environment came with publication of the Merseyside Guidelines
on HIA (Scott-Samuel et al, 1998).
However, that Government’s early pronouncements on HIA
(see Figure 3) (see also DoH Press Office 1998) may have contributed
to present tensions among HIA experts in the UK between those for
whom the ‘process of HIA’ (including public participation) is of primary
importance and those who argue (in the context of an evidence-based
culture) that the methods used should be scientifically rigorous.
3.1.1 Factors affecting the use of HIA in the UK
Table 1 shows these factors that were identified by the Welsh Assembly
Government as affecting the use of HIA. However, reading of other
UK literature shows that these factors are generalisable to England
and Scotland.
TABLE 1: Factors affecting the use of HIA and intersectoral working
in Wales (adapted from: Breeze C and Hall R. 2002)
|
POSITIVE/ENABLERS
|
NEGATIVE/BARRIERS
|
| a. |
Recognition of social and economic determinants of health. |
Gaps in the evidence base of the interrelationships between policy
areas. |
| b. |
Evidence in the links between health and policy areas, and easy access
to it. |
Misconceptions of ‘HEALTH’. |
| c. |
Examples of how HIA has been applied and evidence of how it has helped/benefits. |
Lack of awareness and understanding of HIA. |
| d. |
Strategic use of research funding programmes to expand the evidence
base. |
Narrow or ‘traditional’ views in some policy areas. |
| e. |
Major change that leads to a ‘shake up’ of government organisations
and practices. |
Lack of, or outdated, guidance for policy making. |
| f. |
Political commitment to an integrated approach and commitment to follow
it through. |
Business overload resulting in policymakers concentrating on their
own policy field. |
| g. |
Catalysts, including crosscutting themes as facilitators and drivers
for horizontal action by policy makers. |
Tight timescales of some policy developments. |
| h. |
Systems and processes that facilitate working across policy areas in
the early stages of policy development and implementation. |
Language and terminology – ‘jargon’ – in different policy areas/sectors. |
| i. |
Organisational structure and size E. g. Assembly is one organisation
as opposed to being a series of separate Ministerial departments. |
HIA developed as a ‘separate’ theme without thoughts to it becoming
part of wider developments in policymaking. |
| j. |
Improvements in organisational culture, dynamics and working practices. |
Policy and/or organisational ‘silos’ reinforce vertical structures
and hinder horizontal working. |
| k. |
Health featured as high level strategic objective. |
Organisations that are static in terms of changing their culture and
practices. |
| l. |
Capacity/resources for HIA. |
Process failures or lack of processes for screening of policies and
programmes for their relevance to health. |
| m. |
|
Lack of capacity/resources to undertake assessment within the necessary
timescales. |
| n. |
|
Multitude of impact assessment required increases workloads and resistance
to impact assessment. |
The original table produced by Breeze and Hall appeared to list
factors randomly. In consequence, any later attempt to compare and
contrast Welsh and Hungarian factors needs to start by looking for
categories or groupings of factors.
Drawing, in part, on the capacity building framework
for public health developed, tested and applied in New South Wales
(Hawe et al 2000, NSW 2000) and relationship of evidence to policy/practice
(Nutbeam 2001), the following categories can be identified among the
factors listed by Breeze and Hall. These are from the Table 1:
- Evidence (a-d enablers and a-c barriers)
- Political/policy (e-h enablers and d-i barriers)
- Institutional (i-k enablers and j-l barriers)
- Resources (l enabler and m-n barriers).
In reality, these different categories are interdependent. For example,
new evidence may inform policy decisions and subsequent allocation
of resources. Or, a policy decision may determine priorities for research
funding and hence the type of evidence that is then available to policy
makers. In this analysis, policy and political factors appear to be
the most significant block of barriers affecting the use of HIA in
Wales.
3.1. 2 Lessons from the UK experience
A number of preliminary lessons can be drawn from experience in the
UK. These include:
- Examples of areas addressed by HIA include – transport policy
[Scotland], urban regeneration [Scotland], bio-diversity [London,
England], air quality [London, England], an extra runway for Manchester
Airport [England], the EU funded Objective 1 programme [Wales].
- Increasing recognition of the need to do HIA at policy level,
because of the more wider ranging effects, and wider resource
implication of policy compared to programmes and projects.
- The tendency for ‘health’ to be narrowly interpreted by non-health
sector policy-makers, professionals and the general public. Each
policy area is fed by its own jargon and technical terms. These
can act as barriers to intersectoral working (Wales- Breeze and
Hall 2002).
- The importance of seeing HIA in its wider context i.e. the
development and implementation of Government policy. The ultimate
goal is to help people to improve their health and reduce health
inequalities and to use HIA successfully to achieve this (Wales
- Breeze and Hall 2002).
- The importance of building on capacities that already exist
in a country. In Scotland, people doing HIA case studies benefited
from traditions and available infrastructure supporting inter-agency
working and community participation (Scotland - SNAP 2000).
- Longer-term experience in environmental and social impact
assessments suggest that meaningful approaches to and methods
for HIA will emphasise:
- equitable outcomes
- explicitly targeting disadvantaged groups
- enabling the fullest possible participation by those
groups or communities most likely to be affected by any specific
policy, programme or project
- using qualitative as well as quantitative methods
(England - Scott-Samuel 1996).
- That the HIA process can become unnecessarily long if people
are not able to commit full time to conducting an HIA, writing
it up and supporting its use in the relevant policy processes.
- The lack of a statutory requirement for HIA to be carried out
means that it risks not entering the mainstream of non-health
sector institutional and policy processes. It is important to
mainstream the impact assessment concept in processes, systems
and organisational culture. HIA can’t be viewed in isolation.
- Modernisation agendas for public administration and policy
making should underpin HIA by
- being committed to open and inclusive policy-making
- legitimising collaboration across policy areas on cross-cutting
policy themes such as public health and sustainable development
(Wales- Breeze and Hall 2002).
3.2 HIA in the Netherlands
Development of HIA in the Netherlands has been more coherent and systematic,
particularly in the assessment of national government policy.
The history of the development of HIA in the Netherlands
has been well documented (Put et al 2001). Based on expert consultations
during 1993-4, the Minister of Health, Welfare and Sport informed
the Netherlands Parliament during 1995-6 about the main points of
her policy programme. This included developing a methodology for screening
policy proposals made by other Ministries and identifying those that
might impact on public health. The methodology would also support
more in-depth assessment of policy proposals meeting certain threshold
criteria with a view to exerting influence during the official preparatory
process. (Letters 24/126, No.3 and No 14, Public Health Policy 1995-98).
In 1996, the Intersectoral Policy Office was set up
in the Netherlands School of Public Health (NSPH) in order to
coordinate development of the necessary methodology and a sum of 230,000
euro was allocated to implement a plan of action to develop (see Figure
4)
Figure 4: Main objectives of
the Dutch Plan of Action to develop HIA in 1995
- Make an inventory of existing methods
and tools for impact assessment in the Netherlands, as well as
foreign experience.
- Work out methods for estimating the
size and significance of impacts on health of policy proposals.
- Develop procedures for HIA.
- Assess the performance of HIA in practice.
- Investigate the possibilities for
institutionalising HIA.
(Source: Put et al 2001)
Since then, the total annual budget for the IPO has
increased from 230,000 to 340,000 euros, while the sum allocated for
commissioning specific HIA studies has increased from 65,000 to 95,000
euros. The IPO is financed by the Health Ministry but has independent
control over its budget.
3.2.1 HIAs produced or coordinated by the NSPH/IPO
Table 2 summarises the range of policy areas covered under the Dutch
programme described previously.
Table 2: HIAs coordinated or produced by the NSPH
| Year |
Topic |
Subject Screening (S) or Assessment (A) |
| 1996 |
Energy tax regulation (Ecotax)
High-speed railway |
S
S
|
| 1997 |
Tobacco policy (2 reports)
Alcohol and Catering Act
Reduction of the dental care package |
S
S
A
|
| 1998 |
National Budget 1997/Annual Survey of Care
Tobacco policy
Election programmes of political parties
ICES (Operation Interdepartmental Commission for Economic Structural
Reinforcement – 2 reports) |
S
A
S
S
|
| 1999 |
Housing Forecast 2030
Identification of policy areas influencing determinants of 5 major
health problems
Occupational Health & Safety Act
24-hours economy
Coalition Agreement
Employment Policy proposals and health effect screening
National Budget 1999
Regional development policy |
S
A
S
S
S
S
S
S
|
| 2000 |
National Budget 2000 |
S
|
| 2001 |
Housing Policy
National Budget 2001 |
A
S
|
3.2.2 Lessons from the Dutch experience
A number of early learning points can be drawn from review of Dutch
material to date:
- That systematic use of HIA in the development of national
policies is possible and practical.
- The importance of high level political support for HIA,
with transparency between Ministries and Parliament about the
findings and implications of HIA studies.
- The value of starting carefully and building up to more
extensive HIAs.
- The importance of providing adequate funding to underpin
the development of HIA and an annual commissioned HIA programme.
- The importance of developing an extensive network of
experts capable of taking on the conduct of HIA studies.
- However, more evidence is needed on what HIA can add
to policy-making and this can only come from its application and
then from learning from and sharing such experiences.
4. SITUATIONAL ANALYSIS IN HUNGARY
Drawing on and sometimes mirroring experiences elsewhere in Europe
(see sections 2 and 3 above), this section presents a situational
analysis for Hungary. This analysis is based on interviews with key
stakeholders, review of documentation and participation in the policy
process, particularly relating to attempts to adopt a broader understanding
of public health in policy and institutional circles (see 1.2 above).
4.1 Policy context in Hungary (1999-2002)
In December 1999, as part of a round of international events designed
to share experience and innovation on HIA, Hungary hosted a meeting
on HIA. At that time there appeared to be little interest in the Ministry
of Health in the value of HIA and scepticism about its relevance in
the context of Hungarian policy making. By contrast, the Environment
Ministry was developing capacity in the commissioning and use of environmental
impact assessment.
More recently, in May 2002, the newly elected Socialist/Free
Democrat coalition Government took office following a general election.
Public announcements by senior Government figures seemed to commit
the Government to designing and delivering health-driven policy in
all sectors of public administration. This mirrors the range of competency
in health matters set out in the Treaty of Amsterdam of the European
Union. Not without coincidence, Hungary is on track for accession
to the EU in May 2004.
This new approach to healthy public policy will, for
this Government, be underpinned by intersectoral action on health
and continuing reform of public administration in Hungary. Together,
they appear to provide a supportive environment for the introduction
and implementation of HIA.
More concretely:
- a new Public Health Division was established at the Ministry
of Health, Social and Family Affairs in September 2002 with
interest in championing health development
- provision for a regional health development function alongside
Regional Development Committees was included in the National
Development Plan for Hungary submitted to the EU
- the Hungarian Parliament will debate a new National Public
Health Programme sometime in March 2003
- subsequently, further strategic and institutional development
in the areas of health development and Public Health are planned
during 2003-2005.
One of the options under consideration is that HIA can be institutionalised
in the governmental sector through a new background Health Policy
Institute that could be established in relation to the MoHSFA.
4.2 Factors affecting the use of HIA in Hungary
The factors discussed in this section are drawn from interviews conducted
with key stakeholders and analysis of documents in order to contribute
to a situational analysis of HIA in Hungary. Table 3 summarises these
factors.
As with Table 1, the factors presented in Table 3 can
be grouped into four main categories for comparative purposes:
- Evidence (a-c barriers)
- Political/policy (a-d enablers and d-i barriers)
- Institutional (e enablers and j-m barriers)
- Resources (f-i enabler and n-q barriers).
A quick look at table three shows a considerable number of barriers
and far fewer ‘opportunities’ than identified in the UK context. However,
not all stakeholders had an adequate overview of the developments
listed in 4.1 above most of which may facilitate the introduction
of HIA in Hungary.
TABLE 3: Factors affecting the use of HIA in Hungary
|
POSITIVE/ENABLERS
|
NEGATIVE/BARRIERS
|
| a. |
International policy priority for HIA. |
Lack of awareness and understanding of Health and HIA. |
| b. |
New National Public Health Programme. |
Public Health is a too complex issue. |
| c. |
Political commitment to the use of HIA. |
An insufficient evidence base in HIA. |
| d. |
The need for regionalisation and decentralisation together with the
opportunity to the use of HIA in regional decision making. |
The lack of political commitment to follow through policy announcements. |
| e. |
Institutional development in the Ministry of Health and a new
National Institute for Health Development. |
Unwillingness to really address required system level and organisational
level changes, together with immature political culture. |
| f. |
EU accession in terms of potential collaboration with foreign
partners in HIA project. |
Lack of policy process and strategic thinking and short term interest
conflict with long term development. |
| g. |
Possible interest in the Ministry of Finance to consider use of HIA
to identify and assess health ‘cost’ of policy proposals from spending
Ministries. |
Public Health is not an issue in politics. |
| h. |
Stakeholders interested in HIA. |
Lack of political and professional consensus in Public Health Policy. |
| i. |
Other approaches to evaluate health impact. |
There is discrepancy between policy and research. |
| j. |
|
Key stakeholders don’t share information and don’t work in teams. |
| k. |
|
Immature programme management, unclear responsibilities, weak accountability,
poor performance. |
| l. |
|
There is no partnership between health and non-health sectors for HIA,
and weak intersectoral working for health. |
| m. |
|
Conflicting interests in HIA. |
| n. |
|
Lack of capacity (institutional. Human resources, working examples,
guidance or training materials) for HIA. |
| o. |
|
Weak social capital (trust, confidence) for participation in HIA project. |
| p. |
|
Lack of legal framework for HIA. |
| q. |
|
There is too little time available for HIA before decision making. |
4.2.1 Opportunities in Hungary
a. There is increasing recognition by governments of the importance
of HIA and the needs for international collaboration in order to share
experience, best practice and learn from each other. This is reinforced
by the Article 152 of The Amsterdam Treaty for Member States of the
European Community and the World Health Organization’s Health 21 policy
framework for countries in its European region (Pan-European HIA survey,
2002).
b. The government accepted a new National Public Health
Programme in December 2002 for the next decade. One of the priorities
in the Program is capacity building for health development including
capacity for HIA.
c. The newly elected Socialist/Free Democrat coalition
Government says that it is interested in and committed to the use
of health impact assessment and it is a priority to develop capacity
for HIA.
d. The necessity of decentralisation and regionalisation
is intended to re-allocate power more appropriately between national,
regional and local levels. That should happen in Hungary in the context
of EU accession. The EU will allocate resources for regional development
and Hungary needs to prepare it’s infrastructure for this. That will
open up the regional level of decision making, governance and program
delivery, This will provide a new arena for the application of HIA
in decision making processes.
e. The national government established a new Division
for Public Health in the Ministry of Health, Social and Family Affairs,
and recently accepted a new National Public Health Programme. The
Program will have a new background institution for policy analysis-advice,
program management and health development. Capacity building for Health
Impact Assessment and co-ordination of the related tasks is intended
to become a new function of this Institute.
f. EU accession opens up a new perspective for Hungary
in terms of development of the use for HIA. For example, through collaboration
opportunities with EU partners. Participation as a third party in
the SANCO project would provide valuable experience, knowledge and
importantly, potential leverage to develop the required capacity in
Hungary.
g. Previous discussion involving a Ministry of Finance
colleague dealing with social expenditure, showed interest in getting
a better understanding of HIA as a step to considering its possible
use in identifying and assessing policy proposals from spending Ministries
for potential ‘health costs’ and/or ‘added health value’.
h. Interviewed stakeholders and government have positive
attitude to the use of HIA and they are interested to develop capacity
for it.
i. At present, the baseline situation in Hungary
is a lack of obvious capacity for Policy HIA both within the health
sector and outside of the health sector. Some related infrastructure
and resources exist for example in the:
- Local Health Planning Project of the Hungarian Healthy
City and Soros Foundation
- Ministry of Environment and other bodies for Environmental
Health Impact Assessment
- Ministry of Youth and Sport for the impact of the new ‘drug’
law on the users
- Central European University in terms of integrating Health
into EIA in Central and Eastern Europe (Cherp, 2002). However,
Hungary wasn’t included in the latter activity.
4.2.2 Barriers in Hungary
a. There is a lack of understanding or, at best, a passive awareness
that:
- improved health and quality of life comes mainly from economic
and social developments (including good education) and not
from the health sector and there is a need to assess that
development by HIA
- the technical resources (infrastructure and people skills)
for health impact assessment must be developed
- efforts to improve health must involve working in partnership
with other sectors and with local people.
b. Classical public health with its focus primarily on communicable
diseases, secondary prevention and hygiene protection remains important
in Hungary. However, an efficient public health effort must focus
on helping to reduce inequalities especially as Hungary cannot avoid
the impact of modernisation and globalisation. This requires holistic
thinking to develop well-rounded and appropriate solutions.
c. The evidence base to support HIA is lacking or insufficient
and its application is missing or not appropriate. There is a perception
that Public Health research is very weak in Hungary and there is a
serious lack of resources. The evidence base, concepts, models and
examples that would help Hungary modernise its approach to Public
Health is mostly in English and available only for those who can read
it.
d. There is often a lack of follow-through from political
commitment to implementation in Hungary. There may be several reasons
for this. First, politicians gain profile simply from announcing policy
initiatives and do not seem to be so interested in what happens afterwards.
Second, there can be a lack of obvious mechanisms by which policy
can be translated into action.
e. After the political, economical and social changes
Hungary is still in the process of transformation. Based on my interviews
with key stakeholders and research experiences there is a very real
unwillingness to address the need for system and organisational level
changes. This is made worse by a still developing pluralistic political
culture, disempowered institutions and civic society and, at a basic
level, concerns about job security in a period of significant change.
At the same time EU accession and developmental needs will require
new ways of working, new knowledge, skills to fulfil expectations.
f. Since 1989 Hungary had at least 6 National Public
Health Programme and basically no implementation so far. There was
no clear strategic view about public health and no proper planning
for implementation or institutional development. Within one national
governmental cycle we had several ministers, new organisational structures
and functions, new management or no management. At the same time short
term interests of people within a rigid bureaucracy are barriers to
long term development.
g. Public Health comes up the political agenda during
the last election campaign but seems to fade away after the election,
being overtaken by more pressing reactive/emergency concerns.
h. Mirroring other factors mentioned above, stakeholders
don’t share information, and in only a few areas (such as drug prevention)
is there obvious partnership working.
i. As happens elsewhere, policy and research have different
speeds and natures. The lack of commitment to evidence-based policy
and practice does not provide supportive conditions for using research
in decision-making at policy and practice levels. Policy sometimes
seems to be designed as much as a means of spending the Government’s
short-term budget as it is of addressing basic challenges facing the
Government (wealth creation, social inclusion, public health, democracy).
j. Related to point ‘e’, the working culture within
the health sector and especially within key organisations in the public
health field is based on an out of date command and control approach
combined with a strong sectoral, rather than intersectoral orientation.
It appears that the past 10 years of transition have reinforced this
culture causing organisations and individuals to be afraid and suspicious
to share information and to want to work in teams.
k. In the public health field program management skills
are under-developed, responsibilities are unclear, the accountability
of programmes is weak and performance is poor or not well measured.
One of my interviewee told me that “people are not following roles
and regulation in the Parliament either” (for example the enforcement
of the No Smoking in Public Places Law).
l. Hungary has experience of intersectoral working (World
Bank Health Programme projects, Healthy Cities and Regions for Health
Networks) but have not been able to successfully institutionalise
this. Working in partnership with each other requires new way of thinking
and application of new approaches, methods, tools, etc. Health Impact
Assessment potentially provides a concrete and practical way of increasing
commitment by health and other non-health sectors for better health
and quality of life for people.
m. There are different stakeholders and institutions
in different policy proposals and programme and they can have conflicting
interests to carry out HIA.
n. To date, Hungary has not identified clear institutional
responsibility for coordinating the development of expertise and knowledge
in HIA including the production or/or translation of specific guidance
or training documentation on health impact assessment.
o. Social capital (trust, confidence, knowledge) between
agencies and individuals is weak in Hungary. A paradox of the Socialist
period is that it undermined social capital and replaced it with a
system of state dependency and patronage. Hungary is still passing
though its transformation and it may still be too early after the
system change for significant levels of social capital to have developed
again. As HIA and similar participatory techniques become more widely
used and familiar it may help lead to develop strong confidence and
capabilities in represent broader stakeholder views in the development
of policy and programmes.
p. Hungary has a regulation for social, economical and
environmental impact assessment, but no law for HIA.
q. Sometimes there is too short time for any impact
assessment before decision making. This reality is, in part, responsible
for scepticism for using methods like HIA that ‘delay’ decision-making.
What does not seem to be appreciated is that HIA and similar policy-planning
tools can help improve the quality of policy decision making and,
in consequence, improve the effectiveness and relevance of measures
to implement policies.
5. COMPARISON OF FACTORS AFFECTING THE USE OF HIA
IN HUNGARY AND THE EU
In the UK there appears to be a critical mass of factors at a policy
level that will help promote wider adoption of HIA and related methods
at Institutional and other levels. By contrast this critical mass
has not yet been achieved in Hungary. In part this may be because
of a lack of a broader modernisation agenda for Government/public
administration of the kind seen in the UK and elsewhere. Hungary has
a lot of developmental needs to deal with all the barriers in relation
to the application of HIA methodology. Capacity building means working
on several levels: political, strategic, (inter) institutional and
training.
Learning from the Scottish experience shows that several
actions need to be taken in order to have a real chance for developing
health impact assessment and making healthy public policy:
- There need to be a clear understanding of the responsibilities
and the functions of the institutes and organisational structures
in the field of public health and health promotion.
- A cross departmental audit is needed among the Ministries in
order to ‘map’ how much health is in the centre of the policy
making process.
- A system of control (a kind of checklist) has to be developed
to screen policies for potential health impact and then to help
identify the positive and negative effects of the important health
relevant policies.
- If it is necessary, a detailed HIA should be commissioned.
- Case studies have to be shown concerning how previous assessments
managed to prevent damage or harm or produced benefits. Criteria
have to be formed and prioritised which help to select policies
which should be subjected to HIA later on. This method was used
for example in The Netherlands. Responsibility for case finding
would lie within the health sector.
- Every kind of initiative, programme which can have an impact
on the quality of the life of the people has to use a monitoring
system which places health in the centre, and where it is needed
it has to have mechanisms by which we can intervene.
- External audit is needed whether health is considered in policy
making at local, regional and national level (Adapted from SNAP,
2000).
Evidence
The Welsh study found 4 factors supportive of the use of HIA while
none were mentioned by Hungarian stakeholders. In Wales and the UK
generally, there has been for some years a political and policy supported
drive for evidence-based decision making. In turn, this has helped
to generate funding for applied research that can be used to support
decision making. This situation is not the case in Hungary at present.
A problem is that much work on HIA is published and reported in English
but English language (and other foreign language) skills are not widespread
in public administration. Without either improving English language
skills (as is being done in the Military following joining NATO) or
making this English evidence base available through significant investment
in translation, Hungary can’t take advantage of this investment and
learning from abroad.
Political/Policy
The political/policy factors are the most significant category of
barriers in both countries. However, the nature of negative factors
is different in Hungary than in Wales. In Hungary the main problems
are the lack of a transparent policy process, political commitment
to follow through policy announcements, limited means for exploring
and making consensus among sectors and stakeholders around shared
policy priorities, unwillingness to address system and organisational
level changes, discrepancy between policy and research and no priority
for public health. In contrast Wales has the following barriers: narrow
views in some policy areas, lack of policy guidance, business overload,
tight timescales, terminology jargon and HIA is not a part of decision
making. Positively, in both countries there is a political commitment
to the use of HIA and major changes in the policy environment are
supportive factors as well. There are other differences between the
two countries. In Hungary international and national level policy
priorities are positive contributors, while in Wales HIA, as a crosscutting
catalyst for horizontal action, and systems and processes that facilitate
working across policy areas are enablers to the use of HIA.
Institutional
Institutional factors as barriers are almost equally important in
Hungary and Wales as well, but as enablers it is more significant
in Wales. Critically, the Welsh Assembly Government supports the use
of HIA in decision making, among policy implementation agencies health
is a high level strategic objective and different improvements at
organisational level are being made. In Hungary, the Ministry of Health,
Social and Family Affairs established a new division for Public Health
and they have an intention to re-establish a new National Institute
for Health Promotion in Hungary. These developments can be supportive
to the use of HIA at national policy level.
In both countries, important barriers include: weak
horizontal working for health and organisational unwillingness to
change cultural and working practices. In Wales one additional problem
is the apparent failure of processes to screen policies for their
relevance to health. In Hungary immature program management, unclear
responsibilities, weak accountability, poorly monitored performance
and conflicting interest in HIA are all barriers to the use of HIA.
Resources
This category is more significant determinant both as enablers and
barriers in Hungary than in Wales. The Hungarian study found 4 – 4
factors as opportunities and barriers to the use of HIA. Among the
opportunities are EU accession, interest among stakeholders and Ministry
of Finance interest in HIA and other approaches to evaluate policy
proposals submitted by spending Ministries. Among the barriers there
are the lack of capacities and legal framework for HIA, weak participation
and too little time availability before decision making. In Wales
capacity and resources for HIA are enablers to the use of HIA, while
too little time before decision making and increases workloads are
barriers to the use of HIA.
6. CONCLUSIONS AND POLICY RECOMMENDATIONS
The attention paid in this paper to HIA does not minimise appreciation
that Government and public administration in Hungary is confronted
by many significant challenges, especially related to EU Accession.
In that sense, attention to HIA might seem a luxury. However, the
attention given to HIA is important because it helps to illustrate
how these broader challenges are/are not being met.
According to the findings of this research the following
areas should be addressed in developing action at political, institutional
and professional levels
- Hungary needs to deal with those political/policy barriers
that are in the way of developing the use of HIA at national governmental
level. At the same time Hungary can use the support from the international
community and from its own development opportunities as well.
- The Minister for Health, Social and Family Affairs should have
responsibility for reporting to Parliament, at least annually,
on Screening activity and HIAs conducted and-or commissioned and
what subsequent action was taken by relevant Ministries and organisations.
This would also ensure that other Ministries have to account for
corrective actions taken or not taken in response to HIAs
- Hungary needs to address problems located in institutional
cultures, structures and relationships, developing a new attitude
and practice for organisational culture that is supportive of
evidence-based decision making, intersectoral and team working
and involving target population groups
- Key stakeholders, especially public health professionals and
researchers need to develop and promote the necessary evidence
base to support the use of HIA
- In terms of resources Hungary needs to identify and exploit
the opportunities that are available and with realistic budgets,
start to develop capacity to carry out HIA.
Relatedly, experience from elsewhere shows important directions for
the development of HIA in Hungary. For example,
- Carrying out HIA should be an essential part of government
planning and decision making in order to place health in the centre
of the decision making process.
- When facing potential health risk detailed impact assessment
is needed in the interest of eliminating the risk or achieving
a better health gain.
- Carrying out HIA is reasonable and practical, with findings
from a HIA it is really possible to make changes in the decision
making process.
- The HIA should be jointly owned by the health and other sectors.
Determining that a HIA is necessary and initiating it should be
a cooperative decision between the relevant ministries. Negotiating
and implementing the recommended modifications is the responsibility
of the relevant decision makers and government offices.
- HIA can be an integrated part of other impact assessments but
also can be carried out independently. The selection of the necessary
methods and tools depends on the specific task (Adapted from SNAP,
2000).
More specific policy recommendations will be addressed in a parallel
policy briefing paper. The main recommendations are given below.
6.1 Establishing a legal framework for HIA in Hungary
If it is possible, existing capacities should be used and built on
it. It is important to ‘map’ recent impact assessments in the country
taking into considerations their legal regulation. These can be used
as models for forming the regulation for the implementation of HIA.
The Parliament should adopt a resolution as first step
which is essential and necessary for the legitimacy of HIA. For example
there is no document like this in the UK. Only the Environmental Impact
Assessments are regulated by the law. This was created within the
frame of EU regulation. This is why it would be important for Hungary
to take part in a potential EC pilot project (meeting on the topic:
on the Hague conference, 17-23 2002). This could help the formation
of this resolution which would regulate the HIA at the formulation
of those policies which might influence the health status of the people.
6.2 Building capacity
The Hungarian Government should develop mechanisms to consider health
in national policy making, and to support this at all levels. The
assessment of health impacts of policies at national level should
be a priority since the achieved effects are more fundamental and
resource efficient than confining assessment at local or program level.
The Ministry of Health, Social and Family Affairs together
with other sectors (e.g. Ministry of Finance, Prime Minister’s Office)
should support the implementation and use of HIA in Hungary as the
integral part of strategic decision making both at national and at
local government offices and other organizations.
After the necessary preparations a National Advisory
Group should be formed under the New National Public Health Program,
which would be responsible for supervising a Unit dealing with supporting
the implementation and use of HIA in Hungary.
6.3 Institutional development
An independent Research and Development or Health and Public Policy
Unit has to be formed, which is responsible for developing a plan
for implementation and support of technical protocols of HIA in Hungary.
There are several alternatives for positioning such a Unit.
First, the Unit could work within a frame of a civil
organization in order to have opportunities to get resources not only
from the government. This civil organisation should use accessible
and existing experiences and results of both national and international
research projects (e.g. M. Ohr, OSI/IFP research, capacities of the
CEU, Ministry of Environment, others).
Second, funding could be provided for a Unit working
within a background institute of the Ministry of Health, Social and
Family Affairs. This Unit advises on those policies which have to
be examined concerning their potential impact on health, supports
screening within the relevant Ministry and where necessary conducts
or commissions full HIAs. The results are communicated to the Ministry
that is responsible for acting upon the recommendations.
Third, other alternatives are (i) this Unit could be
established as a background Institute to the Ministry of Finance,
recognising that Ministry’s role in determining the shape of the Government’
policy programme (ii) placing the Unit within the Prime Minister’s
Office, as part of a broader drive to modernise Government and public
administration.
7. REFERENCES
Az Egészség Évtizedének Johan Béla
Nemzeti Programja, Budapest, 2002, Miniszterelnöki Hivatal
Birley MH (1996) The health impact assessment of development
projects. Journal of Public Health Medicine, 248-249.
Blane D., Brunner EJ. and Wilkinson R. (1996) The evolution
of public health policy: an anglocentric view of the last fifty years.
In Blane D., Brunner EJ. and Wilkinson R. (eds.) Health and Social
Organisation: towards a health policy for the 21st century. London:
Routledge.
Breeze C (2003, in press) Health Impact Assessment and
government policymaking in European countries: a position report,
draft report before publication
Breeze C., and Hall R. (2002) Health Impact Assessment
in Government policymaking: Developments in Wales, WHO Policy Learning
Curve Series # 5. Welsh Assembly Government and WHO European Centre
for Health Policy: Brussels.
Cabinet Office (2000) Wiring It Up: Whitehall’s Management
of Cross-Cutting Policies and Services. A Performance and Innovation
Unit Report, London: Cabinet Office.
Cherp, Aleg 2002 Integrating Health into EIA in CEE.
22nd Annual Conference of the International Association for Impact
Assessment, 15-21 June 2002, the Hague, Netherlands.
Department of Health (1999) Saving Lives: Our Healthier
Nation. The Stationery Office: London
Department of Health Press Office (1998) Health Impact
Assessments will help measure action in tackling inequalities.
(www.official-documents.co.uk/document/cm43/4386/4386-04.htm1)
Department of Intersectoral Policy, Netherlands School
of Public Health (2000) Plan of Action 2000-2001, NSPH: Utrecht.
European Centre for Health Policy, Health Impact Assessment:
main concepts and suggested approach, Gothenburg consensus paper,
December 1999.
European Centre for Health Policy, Policy Learning Curve
Series, Number 4, Experience with HIA at national policy level in
the Netherlands. A case study, September, 2001.
European Centre for Health Policy, Health Impact Assessment.
Discussion papers, Number 1. Strategies for institutionalizing HIA.
Reiner Banken, September, 2001.
European Union Article 152 (1997) the Amsterdam Treaty.
Brussels: European Commission
Gillies P. (1998) Social capital and its contribution
to public health. In: E. Ziglio, D. Harrison (eds) Social Determinants
of Health: Implications for the Health Professions. Genoa: Italian
National Academy of Medicine, pages 46-50.
Hawe P, King L, Noort M, Jordens C, Lioyd B (2000) Indicators
to help with capacity building in health promotion. Sydney, Australia:
New South Wales Health Department.
Lavis J and Sullivan T (1999) Governing Health. In Drache
D. and Sullivan T. (eds.) Health Reform: Public Success and Private
Failure. London: Routledge.
Leung, S.F. and Wong, C.T. (2002) Health Status and
Labor Supply: Interrelationship and determinants. Hong Kong
University of Science and Technology, 28 May
Levin LS. and Ziglio E. (1996) Health promotion as an
investment strategy: considerations in theory and practice. Health
Promotion International 11(1): 33-40.
Marmot M. and Wilkinson RG. (eds.) (1999) Social Determinants
of Health, Oxford: Oxford University Press.
NSW Health (2000), Capacity Building Framework. Sydney,
Australia: New South Wales Health Department.
Nutbeam D (2001) Evidence-based public policy for health:
matching research and policy need. Promotion and Education 2, supplement:
15-19
Plan of Action 2000-2001, Department of Intersectoral
Policy, Netherlands School of Public Health, Utrecht, The Netherlands
Put GV, den Broeder L, Penris M and Roscam Abbing, EW
(2001) Experience with HIA at National Policy level in the Netherlands:
a case study. WHO Policy Learning Curve Series # 4. WHO European Centre
for Health Policy: Brussels
Scott-Samuel A., (1996) Health Impact Assessment, An
idea whose time has come, BMJ 313, Equity in Health Research and Development
Unit, Department of Public Health, University of Liverpool, L69 3BX
Scott-Samuel A, Birley M and Arden K (1998) The Merseyside
Guidelines for Health Impact Assessment. Liverpool: Merseyside HIA
Steering Group.
Scottish Needs Assessment Programme, (SNAP, 2000) Health
Impact Assessment: Piloting the Process in Scotland, Office for Public
Health in Scotland: Glasgow.
Watson J., Butcher P., Mogyorósy Zs., and Ohr
M. (2001) The contribution of public health to national development.
Findings from an introductory workshop with Hungarian stakeholders.
Workshop report.
Wilkinson R. (1996) Unhealthy Societies: The Affliction
of Inequality. London: Routledge.
World Health Organization (1999) Health 21: The health
for all policy framework for the WHO European Region. European Health
for All Series No. 6. Copenhagen: World Health Organization
Ziglio E et al (2000) Technical Report 2: Investment
for health. For Fifth Global Conference on Health Promotion, Mexico,
5-9 June.
Back to home page